Denial Management
Healthcare organizations should be concerned about both rejected claims and denied claims. The claims rejection management process provides an understanding of the claim’s issues and an opportunity to correct the problems. Denied Claims represent lost revenue or delayed revenue (if the claim gets paid after appeals).
To successfully appeal denied claims, the billers must perform a root-cause analysis, take actions to correct the identifies issues, and file an appeal with the payer. To thrive, a healthcare organization must continuously address the front-end processes’ problems to prevent denials from recurring in the future.
Our experienced and proactive denial management team carefully analyze your remittance advice to identify the root causes of denials, zero pays, claim reversals and meticulously work on them until the claim is closed out.
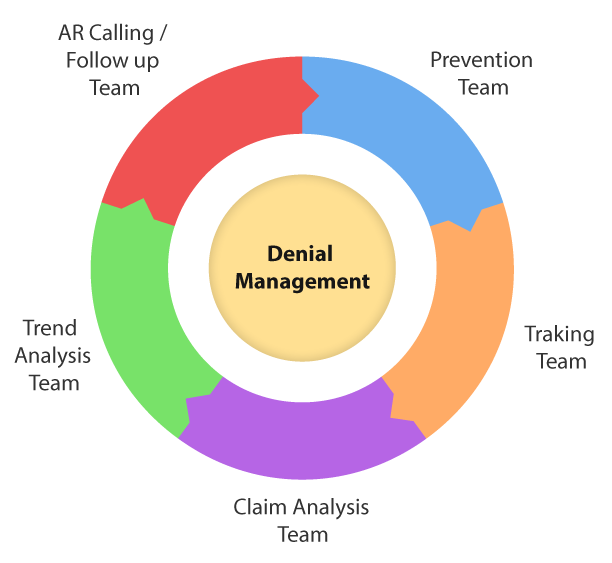
Our Denial Management Solutions
The identified reasons are then categorized and assigned to respective teams for corrective action.
Upon receiving the claims from respective departments, they are resubmitted again for a claim.